Age related macular degeneration or AMD is a progressive, age related disorder that effects central vision. There are two types of AMD — “Dry” and “Wet”:
Dry AMD
Dry AMD occurs when small, age-related deposits called drusen form at the basement of the retina, or the retinal pigment epithelial layer. These age-related changes effect up to 11 million people in the United States. Dry AMD usually requires no treatment, but must be closely monitored as 10 percent of patients may progress to the wet AMD form. Advanced stage dry AMD, or geographic atrophy involves an increased deterioration of the photoreceptor cells. The central area effected may expand over time causing a larger blind spot in vision.
Wet AMD
Wet AMD occurs when abnormal blood vessels form underneath the retina. These vessels break through the retina via the Bruch’s membrane and may leak fluid or blood, causing blurring of the central vision.
What is the cause of Macular Degeneration (AMD)?
AMD is a progressive, degenerative disorder typically found in people over the age of 50, although drusen may be found in younger people.
RISK FACTORS INCLUDE:
- RACE- AMD is most common in Caucasians.
- Family history and genetics- several genes have been found to be linked to AMD
- Smoking cigarettes, obesity, and cardiovascular disease all greatly increases the risk of developing AMD
What are the symptoms of Macular Degeneration (AMD)?
Early AMD changes may not cause noticeable distortion of vision and progression can be slow and subtle so changes may be overlooked at first. Eventually, a person may become aware of:
- Distorted or blurry vision
- Inability to see in dim light
- Difficulty distinguishing color
- Straight lines that appear wavy
- Dark or empty spots in their central vision
Sometimes, people may not be aware of these changes because their other eye sees well, so it is important to test each eye separately by covering one eye at a time when checking vision.
Early detection is key in vision loss prevention. It is important to have a dilated eye exam by an ophthalmologist annually.
If you feel you are experiencing any blurring of your central vision, please contact our office today to schedule an appointment at 215-699-7600.
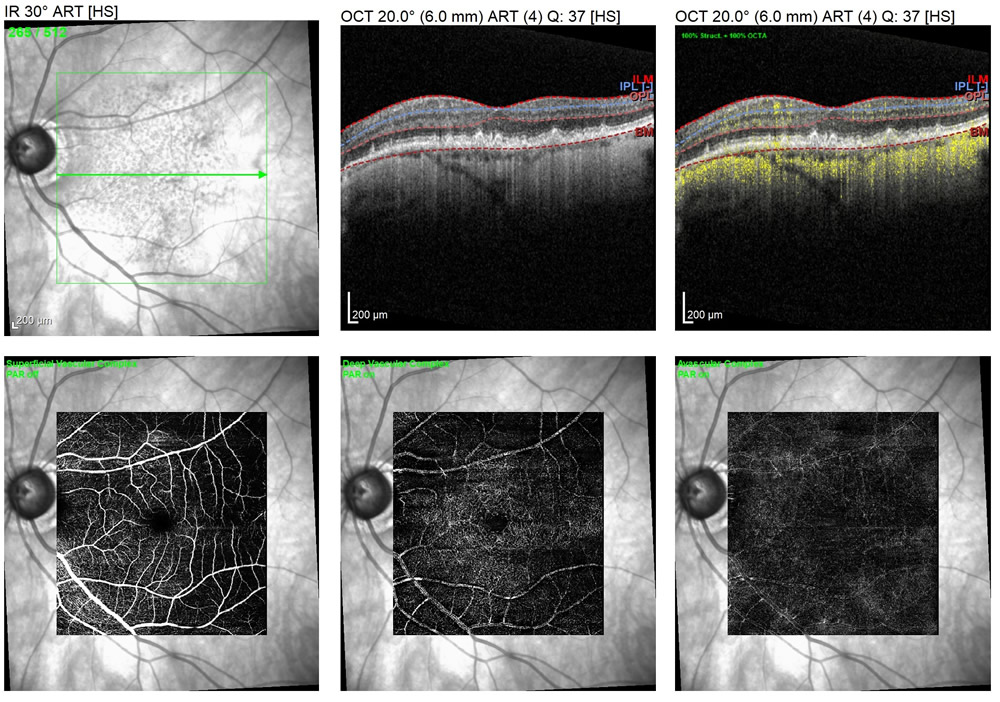
DRY MACULAR DEGENERATION, OR DRY AMD
A multicolor image of the retina with dry AMD shows areas of drusen (yellow spots).
The fundus auto fluorescent image, or FAF image with dry AMD shows multifocal degenerative areas of hyper fluorescence (brighter spots) that correlate with the areas of drusen in the multicolor image. Click here to learn more about fundus autofluorescence, or FAF.
A fluorescein angiogram image of dry AMD shows areas of window defects, or areas of degenerative thinning as well as staining of the dye in the localities of drusen.
An OCT scan of dry AMD shows drusenoid changes in the top right images. The OCT-A scans show blood flow (in yellow) as well as the superficial and deep layers of the retina, and the avascular zone. In the bottom, right image a small, diffuse, ill-defined choroidal neovascular membrane is noted. This eye currently has dry AMD, but with our state-of-the-art testing, we are able to see beneath the surface of the retina to ensure proper ocular health is managed for future sight.
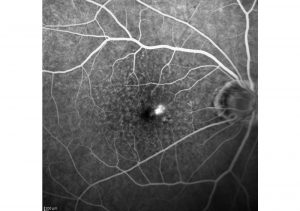
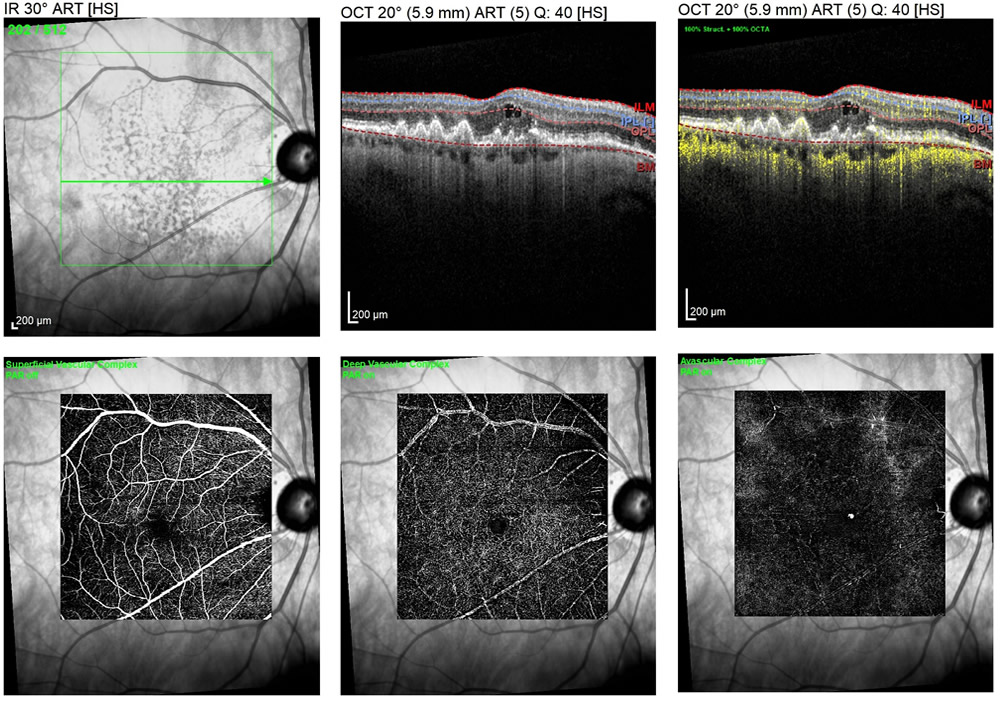
WET MACULAR DEGENERATION, OR WET AMD
A multicolor image of the retina with wet AMD shows areas of drusen (dry AMD changes, yellow spots) as well as a central area of intraretinal fluid.
The fundus auto fluorescent image, or FAF image with wet AMD shows multifocal areas of hyper fluorescence (brighter spots) that correlate with the areas of drusen in the multicolor image, as well as a suspicious central echo in the fovea (center of sharpest vision). Click here to learn more about fundus autofluorescence, or FAF.
A fluorescein angiogram image with wet AMD shows a definitive bright area of leakage, a clear marking of wet macular degeneration.
An OCT scan in wet AMD shows an area of intraretinal fluid in the top right images. The OCT-A scans show blood flow (in yellow) as well as the superficial and deep layers of the retina, and the avascular zone. In the bottom right image, a small, bright area is noted representing an active choroidal neovascular membrane or wet macular degeneration.
What can I expect during a visit to macular degeneration?
After a comprehensive, dilated eye examination is performed by your ophthalmologist, a series of diagnostic tests may be ordered to better evaluate the health of your retina. These tests include, but are not limited to:
- Fundus Photography
- Fundus Autofluorescence (FAF)
- Optical Coherence Tomography (OCT)
- Optical Coherence Tomography Angiography (OCT-A)
- Intravenous Fluorescein Angiography (IVFA)
Along with a comprehensive eye examination, diagnostic testing directly correlates in the assistance of each patient’s individual plan of care. Once diagnostic tests are performed, your physician can better map your retinal needs in order to best preserve your vision.
How is Macular Degeneration (AMD) treated?
Although there is no cure for macular degeneration, there are nutritional supplements, life style changes, and effective clinical treatments available.
One of the most effective treatments for wet AMD is anti-VEGF therapy.
Vascular endothelial growth factor, or VEGF is a molecule generated by the body that causes the abnormal vessels in wet AMD to leak fluid and to bleed into and under the retina. Injections of anti-VEGF drugs into the eye block the activity of VEGF and often result in a decrease in the fluid or blood caused by the abnormal vessels. This procedure only takes moments and is done in the office.
Laser surgery may also be used to treat some types of wet AMD. This procedure only takes moments and is done in the office. After the eye is anesthetized or numbed, the ophthalmologist shines a laser light beam on the specific blood vessels in order to shrink the vessels and stop them from growing. If the blood vessels are in the central macula, or fovea, this option may not be best as it may cause permanent blurred vision in the lasered area. This option is often used when the area of concern may be eccentric to the fovea or not in your central vision. This treatment may need to be repeated over 3-5 years, therefore continual eye exams are important to ensure the treatment continues to be successful.
Your ophthalmologist will discuss with you which course of treatment is best for you.